Postoperational hernias – symptoms, causes, treatment
Postoperational hernias are sometimes called ventral ones; they are characterized by outpouching of the organs of the abdominal cavity or their parts through the defect of the muscular tendinous skeleton, that is located on the anterior wall of the abdomem. Postoperational hernias are developed only in case of suture placing after the operation.
Symptoms
Initial postoperational hernias are easily reduced; pain is absent in this case. When lifting weight, in case of abrupt movement or straining effort some discomfort appears, outpouching is increased. Gradually the outpouching becomes visible, especially in case of coughing or sneezing. Previously pain is dull, later it becomes spasmodic. Disturbance of intestine function is joined to that pain: meteorism, constipation, diarrhea. Urination is sometimes difficult.
A patient becomes passive as a result of intoxication: weakness, vomiting, nausea, sometimes temperature increase troubles a patient. At first small hernia does not cause deformity of the abdomen. Within some period of time discomfort is increased, big hernias can disturb the work of the whole of the body.
In case, if treatment is absent, there is a great risk of development of complications. The most frequent complications are as follows:
- Incarceration of hernia – compression of the contents of the hernial sac in the hernial orifice; due to it necrosis of tissues develop. In 8% of cases this complication causes the lethal outcome.
- Inflammation – in those organs that have got into the hernial sac, inflammatory process starts to develop.
- Coprostasis – stagnation of feces in the intestine.
In case of development of any of these innumerated above conditions pain develops in the area of the pathological centre, the intensity of pain is gradually increasing. Nausea, vomiting, delay of gases, presence of blood in feces, - in case of any of these symptoms one should immediately visit a doctor.
Diagnostics
Diagnostics of the disease in most cases is not difficult. But big hernias should be differentiated from other big formations as they look similar: do not confuse them with lipomas, abscesses, etc. And one should take into consideration that for people, suffering from obesity, only methods of special diagnostics are efficient at the initial stage.
- In case of examination of postoperational scar one can find out asymmetrical outpouching, that is increased during straining. Due to percussion one can hear a tympanic sound, if intestine loops have got into the hernial sac. Omentum or non-caval organ gives a dull sound. Through the cicatricial tissue one can see peristalsis of the intestines.
- Investigation for coughing thrust – after inserting a finger into the hernial orifice, a doctor can feel the thrust during a patient’s coughing.
- USI of the abdominal wall is done to evaluate the conditions of structures: the width of the hernial defect, presence of hernial opening, adhesion, and to exclude partial intestinal obstruction and centres of inflammation.
- X-ray methods, esophagogastroduodenoscopy, MRT, CT are also included into the complex investigation.
- The histological test of tissues, excised during the operation, can also confirm the presence of inflammatory centres, malignant tumours of ovary, etc.
The author’s method of treatment of ventral hernias, using laparoscopy
The laparoscopic access in treatment of ventral hernias is actively used in Europe and the U.S.A. The base of its use are new techniques, that combine the techniques of non-stretched hernioplasty of open surgery and that of the laparoscopic access, that give a possibility to fix mesh implants to the abdominal wall without peritonization (covering by abdomen); it is less traumatic and faster operation, with the excellent cosmetic effect. This technique does not provoke development of seromas and hematomas in the area of postoperational wound and does not require draining of subcutaneous fat, as there is no dissection of tissues in the area of subcutaneous fat.
They think that operations for abdominal hernias are relatively easy, if you take into consideration the technique of it, but at the same time they can be rather complicated in some patients due to the big defect in the abdominal wall or hernial sac and adhesion process in the abdominal cavity. A surgeon should be highly competent to correct these changes, operations are sometimes longer and require the high cost of the used materials. A surgeon, who has no experience of performing on such kind of operations, usually has difficulties while choosing the optimum tactics of treatment-whether it should be laparotomy or laparoscopy? What size of an implant should be chosen, how to fix it properly, how to correct an adhesion process in the abdominal cavity (Fig. 1) without development of additional complications of GIT? In addition to that a surgeon should have knowledge and habits in performing on open hernioplasty and have an experience in laparoscopy.
Indications for laparoscopic access for postoperational ventral hernias
Practically any kind of postoperational hernia can be operated, using miniinvasive access. The more is hernia and the more is BMI, the more there are indications for laparoscopy. The use of this access is accompanied by less blood loss, reduction of seroma amount in the area of hernial sac, absence of the purulent process in the wound and fast recovery.
The choice of laparoscopic technique for the repeated operation after open hernioplasty has some certain advantages. On the one hand, a repeated operation (using laparoscopy) is performed on at another area and at another level of the abdominal wall. On the other hand, practically it is always possible to cover by a mesh the whole of the zone of postoperational scar. As a rule, there is no necessity to remove the mesh, due to it the abdominal wall is not additionally dissected. The possible advantage of the repeated operation, using laparoscopy, is a possibility to find out relapses of hernias, that one has not noticed before; and that relapse can be corrected within the same operation.
For reduction of the number of intraoperation complications and relapses of hernia I have elaborated some certain techniques of operation in case of this disease.
It is important! The peculiarities of performing on laparoscopic hernioplasty by mesh implant in case of postoperational ventral hernias are the following:
- the use of composite mesh, produced by the world leading producers (Switzerland, U.S.A.);
- the introduction of troacars at maximum far distance from the hernial orifice, using the visual control;
- the use of newest electrosurgical platforms and ultrasound scissors for dissection of vascular adhesion (Switzerland, U.S.A.) and the use of “cold” dissection for dissection of the interintestinal adhesion;
- maximum dissection of adhesion and structures for optimum correlation of mesh and abdomen in the zone of operation;
- preliminary herniorrhaphy ( as much as possible, stitching of the hernial orifice before plasty, using the implant);
- the compulsory overlapping of the hernial defect by mesh implant-3-5 cm;
- covering of the whole of the postoperational scar, even if hernia is localized only at one of its edges;
- the use of combined fixation of the implant (transfascial sutures, tackers-both tytatic, and resorbable).
The use of this technique gives a possibility for a patient to get up from bed and take food next day after operation, even after big hernias, and in a day- to leave the clinic.
Below I am describing the peculiarities of my operation technique in detail
The technique of laparoscopic hernioplasty with the use of mesh implant
The development of new mesh implants has changed the technique of laparoscopic hernioplasty, when implant is fixed to the abdomen, without peritonization (Fig. 1).
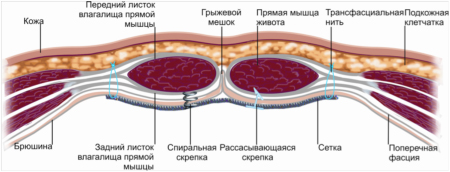
Fig. 1. Positioning of mesh implant intraabdominally (intraperitoneally)
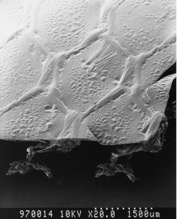 Fig. 2. Composite mesh (Parietex Composite structure).
Fig. 2. Composite mesh (Parietex Composite structure). 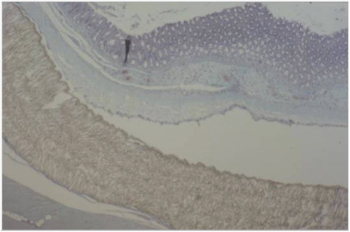 A – Non-adhesive mesh on the basis of polytetrafluorethylene.
A – Non-adhesive mesh on the basis of polytetrafluorethylene. 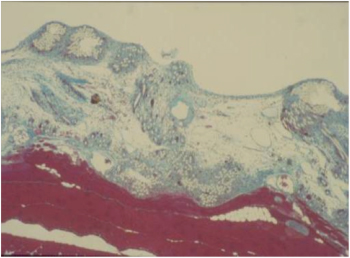 B - Non-adhesive mesh on the basis of collagen barrier.
B - Non-adhesive mesh on the basis of collagen barrier. Fig. 3. Reperitonization of mesh after intraperitoneal implantation.
The latest elaborations in this field have been done by Sofradim Company (Covidien, Switzerland) – composite meshes Parietex Composite with the use of special hydrogel barrier technique give a possibility to implant them without peritonization, with the high degree of safety (Fig. 2). As a result, the composite implantant for the first time has combined antiadhesion properties with the fast and qualitative growth into the adjacent tissues.
Within some period of time a special covering on the mesh is substituted by the abdomen, covering the implant along its length ( Fig. 3).
In my practice I use the technique of three troacars, when at first 10 mm or 12 mm troacar is introduced, then, depending on the anatomic peculiarities of the abdominal cavity, one or two additional 5 or 10 mm troacars are introduced.
It is necessary to use a laparoscope with the angle of survey 30 degrees, as it provides wider visualization of the internal surface of the abdominal wall and organs of the abdominal cavity. The first troacar is introduced into the left subcostal area according to Hasson ( to prevent the injury of the large and small intestines), and through it CO2 is pumped into the abdominal cavity for creating the pressure 12-14 mm Hg. This troacar should always be introduced as laterally as possible, far from the defect on the abdominal wall to provide clear visualization of the edges of the defect. In those cases, when postoperational hernia is located on the midline or to the right, the best option is positioning of three additional troacars on the left side of the abdominal wall.
The points of introduction of troacars should be maximum far from the supposed area of adhesion, taking into consideration the size, localization and number of defects of the abdominal wall; they should be located so, that it will give a possibility to form a triangle around the hernial orifice.
If a defect is of a lesser size, umbilicus can become a port for a laparoscope, and on each side two troacars of lesser size are positioned.
After introduction of troacars and revision laparoscopy of the abdominal cavity, the next stage is dissection of adhesions in the area of hernial orifice. Adhesion develops practically after each invasive procedure in the abdominal cavity. In case of hernioplasty with mesh due to adhesion dissection it is possible to release the abdominal wall around the hernial orifice in order to get space for covering the defect by mesh. There is no need to try to dissect all the adhesions in the abdominal cavity, if there are no clinical manifestations of adhesion obstruction in anamnesis. We should always bear in mind, that it is necessary to dissect adhesions only to provide an adequate covering by mesh the edges of the hernial orifice, from all the sides. If the loops of the large and small intestines are involved into the adhesion process, then I dissect adhesion by the “cold” method and a sharp instrument (Fig. 4).
In case, if large strands of omentum are involved into the adhesion process, I dissect it by means of ultrasound scissors or “LigaSure” instrument (Fig. 5).
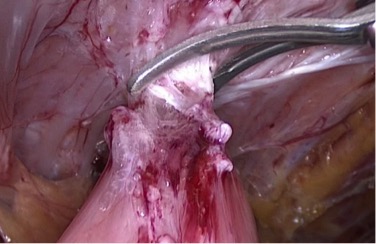
Fig. 4. Dissection of adhesions between the small intestine and the abdominal wall by means of scissors (the “cold” method). |
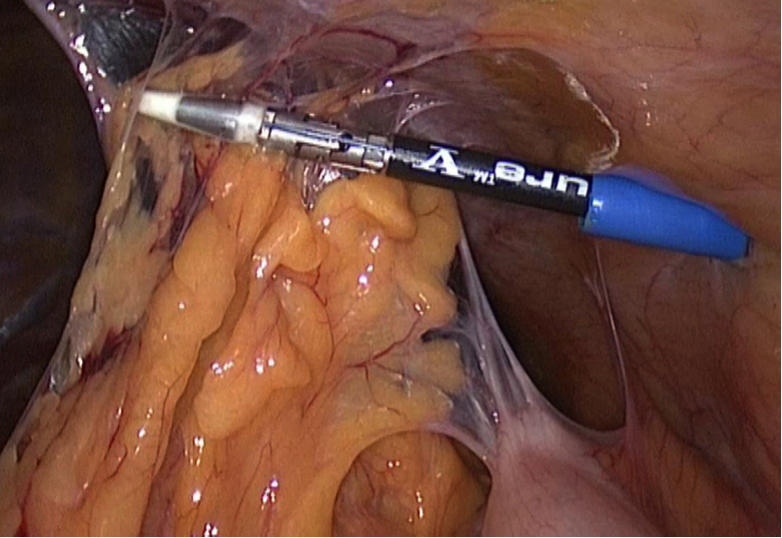
Fig. 5. Dissection of vascular adhesions (strand of omentum) by “LigaSure” instrument. |
At the next stage of the laparoscopic operation it is necessary to determine the maximum exact size of the hernial orifice, as it is necessary for determining the suitable size of mesh and success of plasty.
While determining the size of the hernial orifice, I usually add 6-10 cm to the vertical and transverse sizes. I choose a prosthesis, exceeding those sizes to provide overlapping the defect, it should be 3-5 cm.
Then I always try to decrease the defect of the abdominal wall by means of the partial herniorrhaphy. The main aim of any plasty of the abdominal wall is not only reduction of the contents of the hernial sac and prevention of further increase of the hernial outpouching, but also the restoration of anatomic and functional integrity of the abdominal wall, especially the midline of abdomen. In my own practice I usually use 2 methods of decreasing the hernial defect by means of intracorporeal placing of suture, using needle-holder, and I bind knots extracorporeally through a troacar (Fig. 6) or transabdominally and extracorporeally with the help of “EndoClose” needle (Fig. 7).
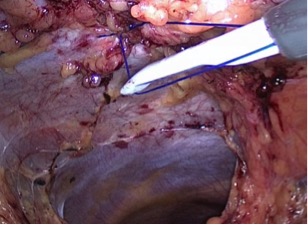
Fig. 6. Laparoscopic herniorrhaphy by means of intracorporeal placing of suture. |
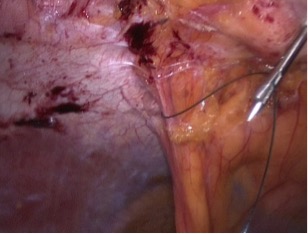
Fig. 7. Laparoscopic herniorrhaphy by means of transabdominal extracorporeal suture with the help of “EndoClose” needle. |
 Fig. 8. Preparing of mesh implant. Additional thread is fixed to the mesh.
Fig. 8. Preparing of mesh implant. Additional thread is fixed to the mesh.Unfortunately, it is possible to do it not in all the cases, as defects can be of big sizes, and it is not possible to bring together its edges.
Then it is necessary to prepare mesh and introduce it into the abdominal cavity. At this stage it is necessary to keep it in sterile physiological solution for 1 – 2 minutes. Additionally I fix thread along the perimetre of the mesh for further transfascial fixation of the mesh (Fig. 9).
It is performed, using 11 or 12 mm troacars. I would like to mark that mesh should overlap the hernial orifice at least 3 - 5 cm in all directions, and this overlapping should be increased proportionally to the size of the defect of the abdominal wall. The necessity of overlapping is due to three factors:
The first one – intraabdominal pressure that can bring an implant into the hernial orifice; the second factor - the more is the mesh, the more will be the area of its contact with the abdominal wall along the edge of the hernial orifice; and due to it its invading to the tissue will be better, i.e. biological fixation; the third factor – the big size of mesh compensates its deformity during fixation and further growth.
Another important moment is a necessity to cover the whole of the postoperational scar to avoid development of an unprotected area of the abdominal wall, where new hernias can develop or relapse will take place.
When the process of implantation of mesh into the abdominal cavity is taking place, it is necessary to decrease pneumoperitoneum up to 9 mm Hg till the final fixation of mesh by stitches is over, then, after fixation by tackers, the pressure again is increased up to 12 – 14 mm Hg.
After placing the mesh implant in the abdominal cavity, its fixation along the perimetre of the defect of aponeurosis takes place by a special device “EndoClose”, one should 3 – 4 cm step aside from the edge of the hernial orifice (Fig. 9).

Fig. 9. “EndoClose” needle (Covidien, Switzerland).
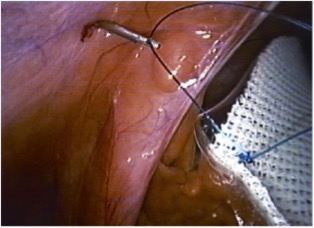 Fig. 10. Implant fixation by means of transfascial suture.
Fig. 10. Implant fixation by means of transfascial suture. At the first stage this fixation is carried out by transfascial stitching (prolene # 0 or 1), thread is conducted through the abdominal wall (thread has been stitched to the implant in advance) (Fig. 10).
Transfacsial fixation is done in the following way: before introduction into the abdominal wall mesh is stitched by П-shaped suture along the perimetre (4 – 6 stitches), and in this way it is immersed into the abdominal cavity. Through 1 mm incision of the abdominal wall ‘EndoStitch” needle is introduced that grasps thread end, and the thread is led out from the abdominal cavity, then the needle again is introduced through that puncture, but in aponeurosis 2 – 3 mm puncture is done, and the second thread is also led out from the abdominal cavity. Then the thread is fixed subcutaneously to aponeurosis by means of several knots, and 1 mm wound on the skin is covered by a special strip.
Another version of fixation is also possible. Through 1 mm incision of the abdominal cavity ’EndoClose” needle with ligature fixed in it is introduced into the abdominal cavity, then we conduct it through the mesh. The needle is led out from the abdominal cavity, ligature is left. We step 5 – 10 mm aside (the puncture by a needle is done, using some angle) from the previous puncture, we again introduce the needle “ EndoClose” into the abdominal cavity, grasp ligature and lead it out onto the abdominal wall, then we grasp ligature by a holder and bind it.
During the second stage mesh is fixed by means of a herniostapler along its perimetre (”EndoUniversal” or “Protack” (Fig.11) .

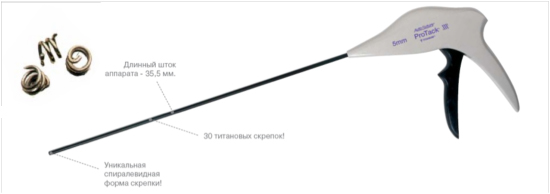
Fig. 11. Instruments for fixation of mesh implants.
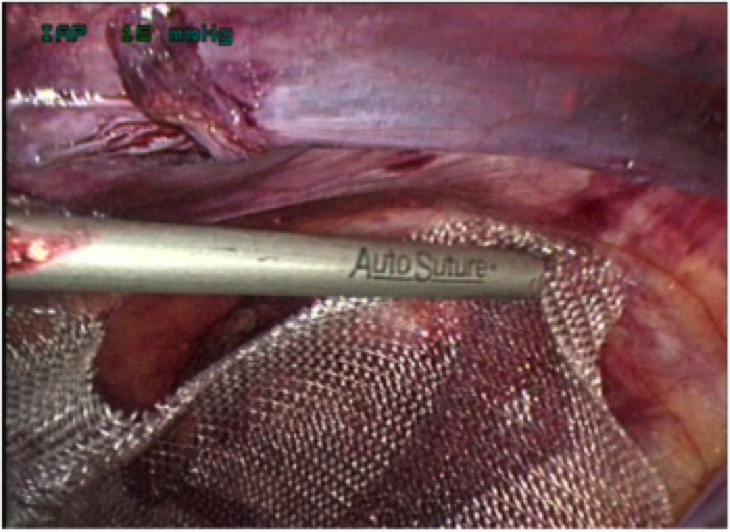 Fig. 12. The stage of laparoscopic operation. Implant fixation by “Protack”
herniostapler.
Fig. 12. The stage of laparoscopic operation. Implant fixation by “Protack”
herniostapler.
 Fig. 13. The stage of laparoscopic operation. Mesh fixation by a herniostapler
with resorbable clips (Covidien, Switzerland).
Fig. 13. The stage of laparoscopic operation. Mesh fixation by a herniostapler
with resorbable clips (Covidien, Switzerland).
I usually use the combined method of transfascial suture and fixation by tackers (Fig. 12). On the one hand, it permits safely to fix an implant, and on the other hand, to have minimum painful syndrome in the postoperational period because of conducting the thread through the whole of the abdominal wall. Resorbable tackers permit to decrease pain in the postoperational period, and the number of relapses is not increased. I use herniostaplers with resorbable clips, manufactured by Covidien Company (Switzerland) (Fig. 13).
In case of oblique hernias on the lateral walls of abdomen, where preabdominal fat is well developed, it is possible to separate the hernial sac, and to perform the plasty, having positioned mesh extraabdominally. If mesh without adhesive covering is used for plasty, it is necessary to peritonize it; for this both endosurgical continuous or interrupted suture is used, and clipping of the edges or placing surgical staples by means of herniostapler. It is not difficult to do peritonization in this case.
For improving adhesion of the remnants of the hernial sac and mesh implant in the postoperational period a patient should wear special compression underwear or a bandage. It provides the best cosmetic effect and is a kind of prophilaxis to prevent seroma formation (accumulation of fluid) in this zone. The term of using a bandage is individual; as a rule, it is 2 – 3 months. Patients, having risk factors (old age, the use of corticosteroids, immunosuppressive therapy, obesity, diabetes mellitus or malignant tumours) and who has surgical risk factors (a big hernia, a long operation, presence of drainage or urinary catheter) should be administered antibiotics of broad spectrum after operation.
Prophilaxis of complications of thromboembolism should be done, taking into consideration risk factors in each individual patient; we compulsory do it, if there are indications.
Pain-killers are required within 2 - 3 days.
Physical exercises are restricted within 4 weeks, then slow swimming and walking, in 2 – 3 months- gymnastics, in 3 – 4 months - serious exercises. Patients should avoid swinging abdomen (in some cases it is allowed in 1 – 2 years after operation).
As mesh implant is thin and light, and it is located under aponeurosis, a patient does not feel it. It is a prosthesis for aponeurosis, but it does not substitude the muscular tissue, that is why at this area the abdominal wall can be thinner.
In conclusion I would like to say that the contemporary mesh implants and various techniques of laparoscopic correction of postoperational ventral hernia permits a surgeon to find an individual approach to treat a patient and to perform on operation with good cosmetic effect and result.




















